Dr. Prosper Meniere who was a devout and observant Parisian physician, described in 1861 the symptoms of the condition that bears his name. He died in 1862 and is probably spinning in his grave because his name is used for almost any condition associated with dizziness and some hearing loss. Meniere’s syndrome is classically defined as a combination of irregular attacks of sensorineural hearing loss associated with tinnitus and vertigo, which tend to occur in pulses. In these 3 classic symptoms a fourth one has been added – the feeling of pressure in the ear with the problem.
The standard form in which this situation arrears, is to a young woman often working under difficult conditions who displays a sense of blockage in one ear and confused, abnormal hearing. Tinnitus may also be observed. These problems are often attributed to a problem with the eustachian tube and treated with a nose decongestant or even antibiotics. The problem disappears until it relapses, leaving probably a somewhat impaired hearing, tinnitus and a feeling of clogged ears. Eventually, usually within the first year of the onset of symptoms, this woman also has an episode of vertigo. This dizziness is not a momentary matter, but lasts for several minutes or even hours and it can be very annoying. More often than not, vertigo is preceded by a period of increased pressure on the ear, worse hearing or louder tinnitus. The surrounding area seems to revolve rapidly, although it may seem that we are the ones who are spinning. Regardless of who seems to be spinning, the person or the surroundings, the sense of non-real movement is annoying and gives the symptoms of vertigo. Usually, vertigo is accompanied by nausea and vomiting.
When vertigo stops, the person that had the episode feels instable – probably for days – and often notes that their hearing has not returned to its previous levels, despite the fact that balance is restored.
Attacks occur in pulses for a period of several months and then seem to disappear, often for about a year before they relapse with the emergence of a relentless, progressive hearing loss and distortion of the residual hearing.
There are many different forms of the disease, but all four symptoms are required (obstruction, hearing loss, tinnitus, vertigo) for the diagnosis and exclude other diseases, such as middle ear disease, especially cholesteatoma and acoustic neuromas. Anyone who has symptoms suggestive of Meniere’s disease should be given full consideration and thorough investigation in an ENT clinic to be absolutely sure that this is actually the problem. Only then can the patient be reassured that nothing serious or life-threatening is behind of symptoms.
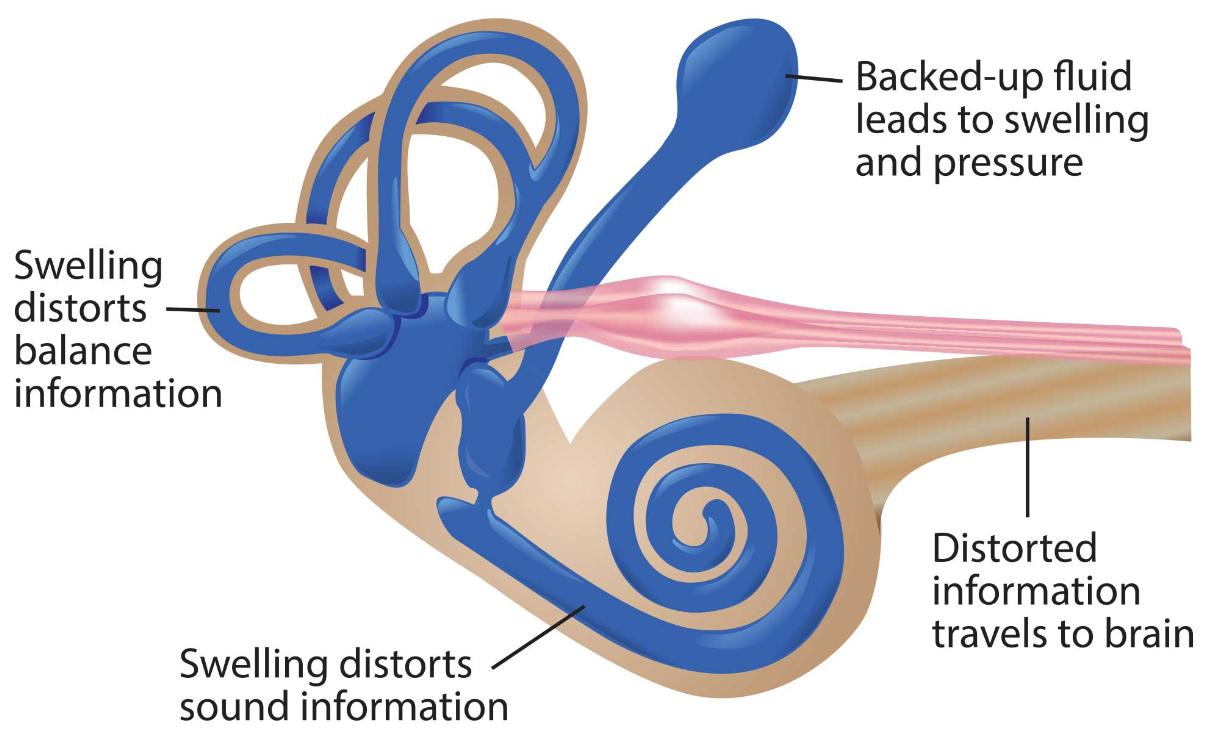
What causes the problem is not known, but it is more common in people with certain personality types, such as intelligent, well organized, clean. This is the same type of personality that often gets migraines and indeed there is a strong correlation within families with Meniere’s disease and migraine through a genetic, chromosomal association. We are not sure of the exact etiology of the Meniere disease, but most probably the blood supply to the inner ear is altered, thus changing the composition of fluids that meet the labyrinth. This in turn causes the symptoms and may be responsible for the frequent worsening of the problem in women during their period, when they develop hormonal changes that affect fluid balance.
If the situation is left untreated, the constant attacks often persist for many years until finally exhausted, leaving behind hearing loss and tinnitus and normal or nearly normal balance. In some cases the other ear may also be infected. The typical image of sensorineural hearing loss is damage to low tones, which first comes and goes but eventually stays in a fixed point. High tones are lost with age and the patient ends up with a hearing loss of about 70dB, which affects all frequencies equally. It is unusual for hearing to become much worse than this level, but the residual hearing is significantly distorted and may not be very useful.
The balance can be evaluated by thermal testing. This test successively introduces cold and hot water to each ear. The difference in water temperature than normal body temperature either triggers (hot) or suspends (cold) the organ of balance in each ear alternately. This causes a false sense of movement (vertigo) and a rhythmic eye movement called nystagmus and may become visible if you follow one’s eyes up close. In Meniere’s disease the affected ear may be initially hyper-reactive, but soon the operation is reduced and this may show in the heat test as a “paralysis” of the canal causing less nystagmus.
Treatment is difficult because the etiology of the disease is unknown. However a thorough examination with the necessary investigation and full explanation of what happens can at least reduce the anxiety of the patient. Anyone not living the experience of a prolonged episode of vertigo finds it difficult to understand how terrifying it can be.
Patients with this condition receive directions to reduce the intake of salt and caffeine, although the full withdrawal did not show any advantage. The only drugs that appear to have some beneficial effect on long-term course of vertigo are thiazide diuretics and betachistine. The acute attack of vertigo can be treated with short-term use drugs such as prochlorperazine and sinnarizine. The latter two drugs should not be used for a long time because they are accompanied by side effects including instability and impaired movement.
There are several operations that can be made in trying to control the vertigo. The mere introduction of a ventilation tube in the tympanic membrane on the affected side seems to help some patients. The intervention in the inner ear (decompression of the sac by removing the bone that covers part of the inner ear – the lymph sac) helps relieve vertigo in 70% of patients for five years or more.
If there is residual hearing, the cross section of the balance nerve (vestibular nerve removal) disconnects the dysfunctional ear from the brain, although it is a major surgery with significant operative risk.
If there is no residual hearing and vertigo is very aggressive, destroying the inner ear (labyrinthectomy) will replace, in the worst of cases, vertigo erratically, which is considered an acceptable alternative for the critically ill.
Treatment of vertigo by injecting aminoglycosides (antibiotics) in the middle ear, to destroy part of the middle ear, has come to the fore again because the newer aminoglycosides have become more predictable in their actions. The aminoglycosides are a group of antibiotics that have the unfortunate side effect to destroy the middle ear. They destroy either the inner and outer hair cells of the cochlea or the balance hair cells, or both, to a lesser or greater extent. These antibiotics when injected in the middle ear it is possible they will enter the inner ear through the round window membrane.
The neomycin almost exclusively destroys the cochlea.
The gentamicin is toxic to most parts of the inner ear related to balance and thus can be used to make a “chemical” destruction of the dysfunctional part of the balance of the middle ear. The surgery is relatively simple and very effective, although there is always a real risk of destruction of residual hearing.
At each stage of the disease there is something that can be done to improve the quality of life of patients, although as the disease progresses it becomes more demanding and the emphasis shifts from stopping the vertigo to preserve hearing.
Above the hair cells there is a gelatinous membrane called the integumentary membrane. One end is glued to bony body in the center of the cochlea. The other end is connected loosely to the organ of Corti on the outside of the outermost outer hair cell. The tips of cilia of the outer hair cells are largely implanted in the lower surface of the integumentary membrane, while the inner hair cells (from which as mentioned come most of the nerve fibers) do not reach the integumentary membrane and stand freely in the inner lymph.
As the sound wave reaches its maximum, outer hair cells located in the area corresponding to the maximum pay a small, normal reinforcement to increase the movement of the base membrane. This internal amplifier makes the inner lymph to move with momentum towards the cilia through the hair cells. If the fluid movement is enough, the cilia are bent and very small channels open at some point near the ends of cilia. Because of the strong electric charge potassium of the inner lymph can then pass through these channels inside the body of the inner hair cells. The entrance of potassium in hair cells causes changes in cell membrane and the release of small quantities of chemicals from the base of the hair cell by neighboring nerve fibers to activate and send nerve impulses to the brain.
The signals pass normally from a relay station to another and go through complex interactions in the brainstem. Approximately 1/5 seconds after detection, the electrical signals reach the auditory areas of the brain (auditory cortex of the temporal lobes) and the sounds are perceived.
At each step of the transmission of sound, the system is configured to maximize the sensitivity of the sound. There is a well-tuned mechanism of the middle ear that produces pressure changes in the cochlea, which eventually form the complex wave that will travel to the brain. In turn, this depends on the delicate structure of the cochlea. There is a very unusual fluid, the inner lymph, and a quite remarkable internal cochlear amplifier. Why? Simply because hearing is an important and very effective warning system. Without good hearing, most mammals would be difficult to survive.